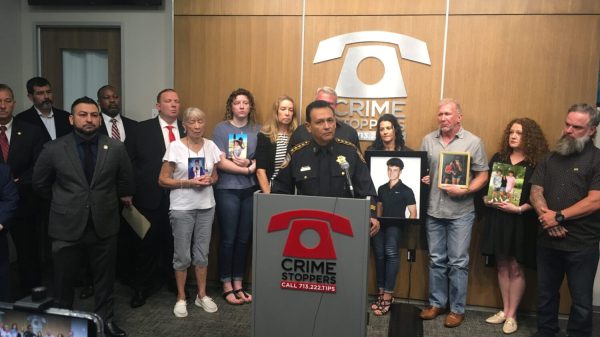
A 2022 Congressional Budget Bill has required the renewal of the enrollment for Medicaid and the Children’s Health Insurance Program (CHIP). In this article, read and find out who will still qualify!
![Children’s Health Insurance Program [Photo: MARCA]](https://s3.us-west-1.amazonaws.com/southarkansassun.com/2023/02/16491635115047.jpg)
Children’s Health Insurance Program [Photo: MARCA]
However, according to an article on CMS.gov, the continuous Medicaid and CHIP coverage is mandated to end in March 2023. A 2022 Congressional Budget Bill authorized the states to remove enrollees who are not qualified for Medicaid and CHIP starting in April. This law says that the enrollment for the coverage must be reassessed and a renewal process must be made for all Medicaid and CHIP enrollees.
READ ALSO: $17.6 Billion Boost In Omnibus Bill For Puerto Rico’s Medicaid Program
How will the enrollment be renewed?
An article on VERIFYThis states that the Centers for Medicare and Medicaid Services (CMS) has required the states to begin the renewal process next year. CMS says that the states must first use the information they have to assess if the enrollees are still qualified for Medicaid or CHIP. If the state needs more information to determine the qualification of an enrollee, a renewal message will be received.
An enrollee reportedly has 30 days to submit the required documents for renewal. During the 30 days, the renewal form must be filled out and returned to the state as soon as possible. If the renewal is ignored, an enrollee will automatically be removed from Medicaid. In addition, if the state determines an enrollee is not qualified, they will be given a notice at least 10 days before they will be removed. During these 10 days, an enrollee can appeal their qualification for the Medicaid coverage.
READ ALSO: Medicare Tax: Definition, Rates, And Why You Pay Them




![Tyson Foods Plant [Photo: Food Manufacturing]](https://southarkansassun.com/wp-content/uploads/2023/08/iStock_1185520857__1_.5e441daa51cca-600x337.jpg)







![Silverado Senior Living Management Inc. [Photo: Los Angeles Times]](https://southarkansassun.com/wp-content/uploads/2023/10/download-6-4-600x337.jpg)

![China's Wuhan Institute of Virology [Photo: Nature]](https://southarkansassun.com/wp-content/uploads/2023/09/d41586-021-01529-3_19239608-600x337.jpg)













![Medicaid [Photo: Commonwealth Care Alliance]](https://southarkansassun.com/wp-content/uploads/2023/02/Medicaid-Questions-Article.jpg)